This document has been made from my memory of a first aid course I attended, from the course handouts, and from a small amount of other material. Do not use this document out of context. See www.fordy.org/firstaid
Incident Management
A-DATA five point plan:
Assess the situation
Deal with any Danger
Assess each casualty. If any isn't conscious shout for help.
Treat casualties in an appropriate order (e.g. unconscious first)
Deal with Aftermath
Casualty Management
“Dr. ABC” primary survey:
... for dealing with any casualty or case of sudden illness.
|
|
Danger |
Are you or the casualty in any? |
|
|
Response |
Is the casualty unresponsive? If so, shout for help. |
|
|
|
Talk to them using their name / give a direct instruction / shake shoulders. |
|
|
Airway |
Is the casualty's airway open and clear? |
|
|
|
Hold their head back (so tongue isn't a blockage), mouth open and look inside. Remove any obvious obstructions. |
|
|
Breathing |
How is the casualty's breathing? |
|
|
|
Place your ear over their mouth looking along the chest for 10 seconds. |
|
|
Circulation |
Only progress to this step if the casualty is breathing fine. |
|
|
|
Can you see, hear or feel breathing, coughing, movement or any other signs of life? Is there any severe bleeding? You might check the pulse rhythm. |
Response levels. AVPU = Alert / responds to Voice / responds to Pain / Unresponsive
So if they don't respond to you shaking their shoulders they are unresponsive, so you must do the ABC.
Breathing.
- If they are breathing but with any difficulty or you have any doubts, get them off their back (where tongue blocks throat, chest weight impedes inspiration, saliva builds up) into the recovery position (where breathing is much easier). See section below on the recovery position.
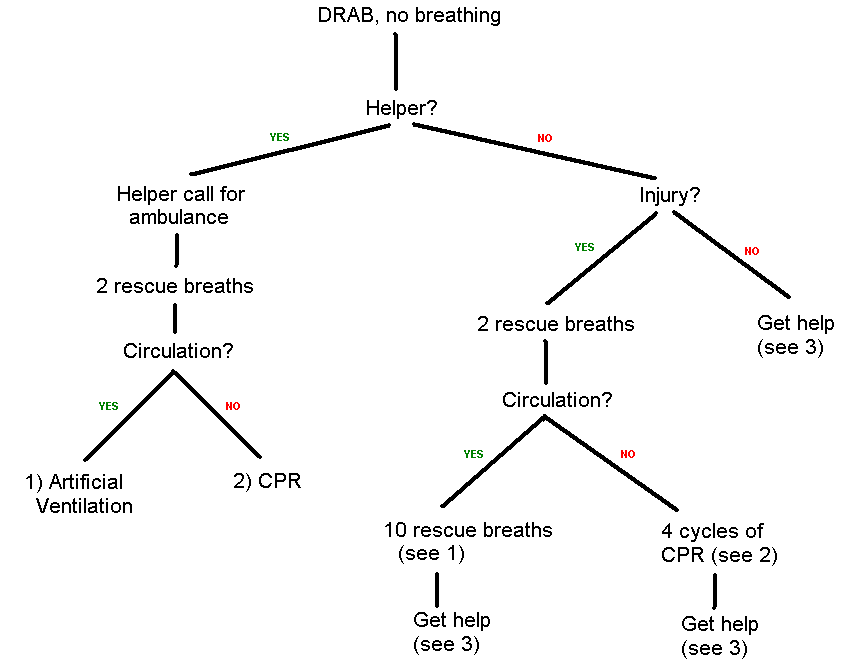
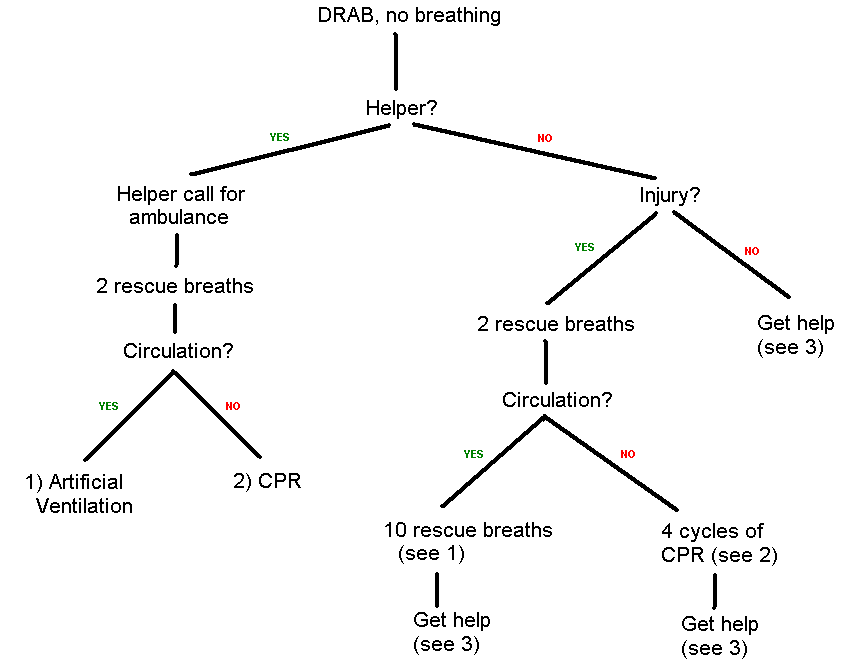
- If they are not breathing, time is of the essence. There are a few different procedures to follow depending on:
is there someone to get an ambulance?
if not, was it an injury (includes drowning, choking, etc.), or a spontaneous collapse?
does the casualty have circulation?
This flow chart explains it:
Non-Breathing Casualty
Checking for Circulation
Apparently, checking for a pulse is not reliable when done by first aiders with this level of training. It is tempting to try to second guess the people who have designed this procedure and try to work out what they were thinking, etc. Should I take the pulse just to be sure before CPR? Maybe they want a bias towards false positives because statistically you can't help the negatives (casualties with no circulation) much anyway? Etc. BUT, instead of all that I think it's best just to trust them. So ...
Someone with circulation may look alert in their eyes, e.g. eye movement. Their may be other signs of life like breathing, coughing or small movements. In contrast, someone without circulation will have cold and clammy skin, and look pale. To put it bluntly, they will look dead.
Don't be over-reluctant to diagnose no circulation and start CPR. The following is taken from the first aid section of the BBC website (Source: http://www.bbc.co.uk/health/first_aid_action/getting_started_pg3.shtml):
Misconception 7. "If you perform CPR on someone who has a pulse you can damage the heart."
The evidence is that it isn’t dangerous to do chest compressions on a casualty with a pulse.
1) Artificial Ventilation
If there is a face shield available, use it. You can improvize with a piece of plastic (e.g. carrier bag) with a smallish hole punched through.
Tilt casualty's head backwards (so the tongue doesn't block the throat) and pinch their nose. Take a full breath. Place your lips around casualty's mouth making a good seal and blow in gently until you see the chest rise. 2 seconds for full inflation. Deflation takes up to 4 seconds. (Hence) 10 rescue breaths per minute. After every 10, check again for circulation and repeat. Continue until help takes over or the casualty starts breathing.
If the chest doesn't rise, check that: the head is tilted back far enough, the seal is firm enough, the nostrils are completely closed, and the airway is not obstructed. If you can't clear any obstructions and get the chest to rise, go straight to CPR.
For mouth-to-nose, you have to allow the mouth to open to let the air back out again after each breath.
2) Cardiopulmonary Resuscitation (CPR)
Feel where the rib cage tapers up to the sternum. Place two fingers on the sternum and then place the heel of your hand alongside the fingers, so that your hand is perpendicular to the casualty. Place your other hand on top and interlock the fingers. Position your body right above your hands so that the force will come mainly from allowing your bodyweight to fall down – with the force being transmitted through straight arms and shoulders. This is not a triceps exercise.
Depress the chest to one third of its depth 15 times, at a rate of 100 compressions per minute. “1 and 2 and 3 and ... 14 and 15”. Then immediately and quickly but correctly apply 2 rescue breaths. And immediately but correctly start the cycle again and repeat until help takes over. (15 : 2 : 15 : 2 : 15 ...)
Only push down hard enough to achieve the required compression and keep up the required rate. You are trying to force blood around the body not break the ribs (though this may well happen anyway).
It is unlikely that the casualty will recover without defibrillation (done by a paramedic), so do not stop CPR to check them. Just keep going until the paramedics take over.
3) Getting Help
If you send someone for an ambulance, make sure they emphasize that the casualty isn't breathing (you might also know immediately that there is no circulation). Make sure they return to you afterwards.
If you have to go for an ambulance yourself (all routes on the right half of the flow chart above end with you calling for help), tell the operator that you know CPR so that they know to get you off the phone and back to the casualty ASAP. When you do return, do Dr. ABC again; don't make too many assumptions based on your previous assessment. In particular, even if they did have circulation before, they may not any more. N.B. you will now of course be following the left half of the flow chart above.
Recovery Position
For an Unconscious Breathing Casualty. Purpose: to maintain breathing.
Procedure
N.B. If there is already a problem affecting the casualty's breathing (e.g. they're vomiting) you may need to hurry and so skip or postpone some of these steps.
Remove their glasses and empty their pockets.
Straighten their legs. Place the arm nearest you at approximately right angles to their body with the palm upwards. Joint inflexibility may prevent it from touching the ground at the full 90°. (Don't lever it down!)
Bring their other arm across the chest. Place your palm against theirs and hold their hand against their cheek until step 5 is completed.
Kneel next to them so that they won't roll too far. Hold their far leg just above the knee and lift it up so the knee joint flexes. Then pull the knee so they roll towards you.
Adjust their upper leg (if necessary) so that the hip and the knee are both approximately at right angles. The casualty should be in the position indicated by this diagram:

Diagram from the HSE's What to do in an emergency http://www.hse.gov.uk/pubns/indg347.pdf
Draw their chin forward and tilt their head back.
Check they are still breathing.
Feel from head to toe, including underneath limbs and torso, to check for major bleeding. If there isn't any you can now go for an ambulance.
Once the ambulance is called, continue checking DRABC. To help the professionals, there are various things you can take note of regularly, including the response level and the inspiration and pulse rates (typically 16 and 60-80 per minute respectively) and strengths. (Pulse is taken at the neck of an unconscious casualty, and the wrist otherwise.)
Shock
Shock is where not enough oxygen is getting to the tissues of the body. It's caused either by failure of the pump (heart attack, angina) or by a reduction in the volume of circulatory fluid (internal or external bleeding, serum loss through a burn, diarrhoea, vomiting).
The remainder of this section on shock is quoted from the course notes:
Recognition
At first:
A rapid pulse.
Pale grey skin (esp. inside the lips).
A fingernail or earlobe, if pressed, will not regain colour immediately.
Sweating and cold, clammy skin, (because the sweat doesn't evaporate).
As shock develops there may be:
Weakness and giddiness.
Nausea, and possible vomiting.
Thirst.
Rapid shallow breathing.
A weak 'thready' pulse.
As oxygen supply to the brain weakens:
The casualty may become restless, anxious and even aggressive.
The casualty may yawn and gasp for air.
The casualty will become unconscious.
Finally the heart will stop.
Treatment
Treat any cause of shock you can remedy (such as external bleeding).
Lay the casualty down, keeping head low
Raise and support the legs
Loosen tight clothing
Insulate from the cold (ideally blankets under and over the casualty)
Send for an ambulance
Maintain breathing and pulse checks until ambulance arrives
Reassure constantly
If they complain of thirst, moisten their lips with water.
Do not:
Let the casualty move unnecessarily, eat, drink or smoke.
Leave the casualty unattended.
Apply heat to the casualty.
Major Bleeding
(For minor bleeding, first aid is simply to prevent infection. Wash with plenty of water, perhaps swabs, etc. Probably put a plaster on although these days people can even be allergic to plasters.)
The 6 point plan of treatment is quoted from the course notes:
For a wound with nothing embedded:
Remove clothing to expose the wound, and apply direct pressure.
Maintaining the pressure, raise and support the injured part.
Unless it's a problem related to or affecting the airway or breathing, lay the casualty down (preferably on a blanket), with legs raised and supported to treat for shock.
Bandage dressing firmly in place, but not so tightly that you cut off blood supply to limb.
Get appropriate medical help. If bleeding is severe dial 999 for an ambulance, keeping the injured part raised and supported.
If bleeding continues through the bandage, secure another dressing over the top. If blood comes through the second dressing, remove both and apply a new one carefully, checking you have the wound properly covered.
For a nose bleed: Casualty should sit down, lean forwards and pinch the soft part of the nose (so they can't breathe through it). Let go after 10 minutes and then 20 minutes to see if bleeding has stopped. If it still hasn't stopped after 30 you should seek medical help.
Disorders of the Heart
All arteries are susceptible to narrowing and blockage. Obviously this is most serious when it affects the coronary arteries, for which (roughly speaking) narrowing and blockage are angina and heart attack respectively. And obviously the two problems are related because (for one thing) a narrow artery is easier to block.
Angina
Caused by exertion or excitement; the extra demands on the heart are not catered for by enough coronary blood.
Possible Symptoms:
Gripping chest pain.
Pain spreads to the (left) arm, jaw and/or hand.
Shortness of breath.
Weakness.
Treatment:
Help the casualty sit down. Reassure them and make them comfortable, perhaps loosen clothing. If they have medicine for angina, help them take it. The pain should soon ease with rest (and the medication). If it doesn't, assume a heart attack and dial 999.
Heart Attack
(Do not confuse with cardiac arrest, which is any stoppage of the heart - i.e. simply, no circulation. Cardiac arrest might result from a heart attack.)
Heart attacks can be more sudden than angina, and not necessarily caused by any obvious trigger. The possible symptoms include all those of angina. In addition:
The vice-like heart-centred pain does not ease with rest.
'Warning' pain like severe indigestion.
A sense of impending doom or total fear.
'Ashen' skin, blueness at the lips.
Irregular, weakening pulse.
Collapse, often without warning.
Once you suspect a heart attack, not angina, and have called 999 (“I suspect a heart attack”), you can offer them an ordinary aspirin if available; tell them to chew it slowly. Maintain constant DRABC checks and follow the relevant procedures already detailed (unconscious => recovery position, not breathing => rescue breaths, etc.)
Epilepsy
Minor Seizure
Sometimes known as an “absence”. The person may freeze, fidget, make funny noises, or just stare. It may look like daydreaming. Call their name. If they don't respond or weren't aware they were daydreaming, it was probably a seizure. Because of this unawareness, they may not know they have epilepsy, and they may not believe they just had a seizure. Make sure they are away from danger both during and after (which can be anything from a nearby hot drink to a major road they want to cross).
Major Seizure
Five phases:
'Aura' phase – they may have a sense (perhaps a taste or smell) unique to them that warns them of an impending seizure.
Rigid phase – they will probably fall over. I personally would try to catch and slowly lower them to prevent injury.
Convulsions phase – they may also salivate and lose bladder and bowel control. Continue trying to prevent injury; cushion the head, and loosen neck clothing for example. But do not restrain. If this is their first ever major seizure call an ambulance.
Unconscious phase – this is the most dangerous phase. They may just be in a daze, but if they are unconscious maintain constant DRABC checks (following the relevant procedures already detailed) and put them in the recovery position. This should only last a few minutes, certainly less than 10, otherwise call an ambulance.
Conscious phase – they will be exhausted, perhaps embarrassed, and need full time attention until they are fully recovered. If they go into another seizure, call an ambulance.
Burns and Scalds
Burn; a hot dry heat.
Scald; hot oil or water, or steam.
Immediately apply cold running water (or whatever's available) for 10 minutes. Then wrap in cling film or a clean tea towel or other suitable material. (You don't want it to disintegrate or make fluff or stick to the wound.)
The patient should end up (how quickly depends on the severity) in hospital if:
the blister is bigger than the size of the palm of their hand, OR
the red patch is bigger than 5 x the size of their palm, or is a band all the way around a limb.
N.B. Never burst blisters, pick scabs, etc.
Sunburn: cool them down, cover them up, and give them plenty to drink (water based!)
Broken Bones
Potential symptoms:
swelling
pain that gets worse with movement
odd angle/shape
reduced movement
cracking sound
impact mark, later bruising
shock ... if the patient shows any symptoms of shock, and deteriorates at all, it may be internal bleeding; call 999.
Treatment: Support and immobilize
Limbs – you can put padding underneath, tie legs together or improvize a sling.
Spine or neck – make sure they don't move (hold them even).
Rib or jaw – have them sit (not lie) to minimize breathing difficulties (as for all airway/breathing-related injuries) and for the same reason consider minimizing their talking (e.g. with yes/no questions)
They will need taking to hospital somehow, typically by dialling 999 for an ambulance. Don't let them have anything to eat or drink.
Conscious Choking
Bend casualty forwards so that head is lower than chest.
Encourage coughing.
Give up to 5 back slaps.
Then give up to 5 abdominal thrusts.
If someone else is available, have them call an ambulance by now at the latest.
Repeat the alternating 5 back slaps and 5 abdominal thrusts.
If they become unconscious, start DRABC as described above. Do check for breathing, since unconsciousness can relieve a throat muscle spasm. If they still aren't breathing, choking counts as an injury not a spontaneous collapse (for the above flow chart). It is then likely you will have to follow the procedure described above for when rescue breaths fail to make the chest rise.
Back Slap – a sharp blow between the shoulderblades from the flat of your hand, just after a shout to the casualty “ready, cough!”, followed each time by checking to see if the blockage is clear.
Abdominal Thrusts
Stand behind the casualty. Make a fist (the equivalent of a 'thumbs up' sign but where the thumb is clenched back down onto the index finger). Place the fist between the navel and ribcage, with the thumb 'going first'. Wrap your other arm around them and put the hand on top of the fist. Pull sharply upwards and inwards, only transmitting force through your fist; don't squeeze them with your arms. After each one check to see if the blockage is clear. N.B. If you do any abdominal thrusts, the casualty should go to hospital even if the blockage is cleared.
Extras
Asthma - Allow them up to 2 puffs every 10 minutes of their own medication. As already stated, one of the best positions for promoting breathing is sitting on a chair, leaning forwards.
First Aid Kits - If you are to be in a specific situation as 'the' first aider, two items for your own protection to have in the first aid kit are gloves (the disposable type) and a face shield.
For the record, breathing ==> circulation, but circulation =/=> breathing.